Understanding the full scope of the dental implant process empowers you as a patient. From consultation to crown, each stage plays a critical role in ensuring a stable, natural-looking, and long-lasting result.
Table of Contents
Introduction: Why Understanding the Steps Matters?
What Is a Dental Implant Procedure?
Stage 1: Initial Consultation and Clinical Evaluation
Stage 2: 3D Planning and Case Simulation
Stage 3: Placing the Dental Implant
Stage 4: Bone Healing and Osseointegration
Stage 5: Connecting the Abutment
Stage 6: Fixing the Final Restoration
Post-Procedure Healing and Aftercare Tips
What to Expect During Implant Recovery?
Managing Potential Risks and Complications
Final Words
Introduction: Why Understanding the Steps Matters?
Embarking on a dental implant journey can feel overwhelming if you don’t know what to expect. From fear of surgery to questions about healing time, the process can create anxiety. This blog provides an in-depth walkthrough of each phase—from your first appointment to receiving your permanent crown—so you can make confident, informed decisions about your smile restoration.
What Is a Dental Implant Procedure?
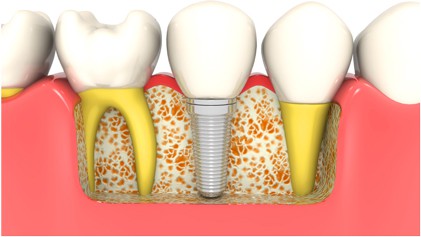
A dental implant procedure is a multi-stage treatment designed to replace missing teeth using a biocompatible titanium fixture that fuses with the jawbone. The implant functions like a natural tooth root and supports a crown, bridge, or denture.
The procedure is typically spaced out over several months to allow for optimal healing and precision. It is suitable for single-tooth replacement, multiple missing teeth, or even full-mouth rehabilitation using All-on-4 or All-on-6 techniques.
Stage 1: Initial Consultation and Clinical Evaluation

The process starts with a comprehensive consultation to evaluate your oral and general health:
- Medical and Dental History Review: Identifies any health conditions (like diabetes or heart disease) that may impact healing.
- Radiographs and 3D Scans: Tools like CBCT help assess jawbone quality and identify nerves, sinus cavities, and bone density.
- Oral Exam: Evaluates gum health, signs of periodontal disease, and the condition of existing teeth.
- Discussion of Goals and Options: Tailors a personalized plan that meets your esthetic and functional expectations.
If bone volume is insufficient, your dentist may recommend grafting or sinus lift procedures to create a stable foundation.
Stage 2: 3D Planning and Case Simulation
Modern implant dentistry heavily relies on digital precision. At this stage, your dentist:
- Uses 3D models and software to simulate implant positioning
- Designs a custom surgical guide to ensure accurate implant placement
- Selects the right implant type, size, and depth based on jaw anatomy
- Reviews different implant brands such as Nobel Biocare, Straumann, and Osstem, which influence healing time and integration
This step minimizes surgical risk and optimizes both esthetics and function.
Stage 3: Placing the Dental Implant

This is the surgical phase, where the implant is inserted into the jawbone:
- Local Anesthesia or Sedation: Ensures a pain-free procedure
- Gum Incision: A small flap is created to access the bone
- Drilling: A carefully measured hole is drilled into the jaw
- Implant Placement: The titanium post is inserted
- Closure: Gums are stitched or a healing cap is placed
For patients with dental anxiety or those undergoing multiple implants, conscious sedation is available. This involves administering mild sedatives either orally or intravenously to help the patient feel relaxed while remaining awake and responsive. Conscious sedation significantly reduces anxiety, enhances comfort, and allows for a smoother surgical experience.
The procedure is quick and typically completed in 30–60 minutes for a single implant. Patients usually report minimal discomfort.
Stage 4: Bone Healing and Osseointegration
This critical healing phase determines the long-term success of your implant:
- Osseointegration: Bone gradually fuses with the implant surface, anchoring it securely
- Healing Time: 3–4 months for the lower jaw; 4–6 months for the upper jaw
During this phase, you may receive a temporary prosthesis and will be asked to follow dietary and oral hygiene instructions to promote optimal healing.
Stage 5: Connecting the Abutment
Once the implant is securely integrated with the bone, it’s time to place the abutment:
- Exposure of the Implant: The gum is reopened if needed
- Abutment Fixation: A connector post is attached to the implant
- Impressions: Digital or physical molds are taken to create your custom crown
Some systems allow for immediate abutment placement to reduce surgical visits.
Stage 6: Fixing the Final Restoration
The final prosthesis—your new tooth—is attached to the abutment:
- Material Options: Common choices include zirconia, ceramic, and PFM (porcelain-fused-to-metal)
- Customization: The crown is shaped, shaded, and polished to match your existing teeth
- Final Fit Check: Ensures your bite is aligned and your smile looks natural
This crown is strong, esthetic, and functional, completing your tooth replacement.
Post-Procedure Healing and Aftercare Tips
After each surgical stage, especially implant placement, aftercare is essential:
- Take medications as prescribed (antibiotics, pain relievers)
- Apply cold compresses to manage swelling
- Eat soft foods and avoid hard, spicy, or hot meals for a few days
- Maintain gentle brushing and rinsing routines
Return to daily activities is usually possible within 24–48 hours, although full healing takes weeks to months.
What to Expect During Implant Recovery?
Recovery symptoms are usually mild and manageable:
- Swelling and slight bruising around the surgical site
- Tenderness or pressure during chewing
- Temporary diet restrictions
- Minor bleeding or oozing for the first 24 hours
Most patients report that discomfort is less than anticipated and well-controlled with prescribed medication.
Managing Potential Risks and Complications
Dental implants are extremely safe when performed by trained professionals. Still, some risks include:
- Infection: Prevented through aseptic technique and antibiotics
- Nerve or sinus involvement: Avoided using precise 3D planning
- Implant failure: Reduced by choosing premium implants and following healing protocols
- Peri-implantitis: A gum infection controlled with hygiene and regular reviews
Regular follow-ups and proper maintenance drastically lower these risks.
Final Words
Understanding the full scope of the dental implant process empowers you as a patient. From consultation to crown, each stage plays a critical role in ensuring a stable, natural-looking, and long-lasting result. Partnering with a skilled implantologist ensures the experience is efficient, safe, and tailored to your needs.
Book Your Implant Consultation with 4 Squares Dentistry
At 4 Squares Dentistry, we deliver advanced dental implant care guided by compassion, accuracy, and experience. Led by Dr. Aesha Imran Syeda, MDS, our clinic combines modern digital tools, globally trusted implant brands, and personalized treatment protocols.
✅ 3D Digital Planning & Guided Surgery
✅ Trusted Brands: Nobel Biocare, Straumann, Osstem
✅ 25+ Specialists and Full-Mouth Implant Solutions
✅ Medavakkam | Gowrivakkam | Madipakkam | Poonamallee High Road
✅ Over 10,000 Happy Smiles Delivered
Schedule Your Consultation
🌐 www.4squaresdentistry.in
📞 +91 73052 22044
✉️ admin@4squaresdentistry.in
About The Author
Dr. Aesha Imran Syeda, MDS
Founder & Clinical Director, 4 Squares Dentistry

