Gum Diseases: Bringing Them Under the Scanner
How often have you noticed your gums while brushing your teeth? How often have you cared for that part of your mouth that holds your teeth in place and contributes to a great smile?
Statistics say that nearly 47.2% of all adults aged thirty and above have some form of gum disease. Another interesting statistic says that gum diseases (or periodontal diseases) increase with age. 70.1% of adults above 65 years are said to have periodontal diseases. Men are more susceptible to gum diseases than women, with statistics standing at 56.4% men versus 38.4% women. These numbers underline the prevalence of gum diseases and the lack of gum care.
In this article, experts from 4 Squares Dentistry, the renowned dental clinics in Medavakkam and dental clinic in Gowrivakkam, explain periodontal diseases, the causes, and symptoms. Read on further to increase your awareness about these dental diseases.
Also Read: Cosmetic Dental Treatments For A Smile Makeover
Gingivitis & Periodontitis: A Closer Look
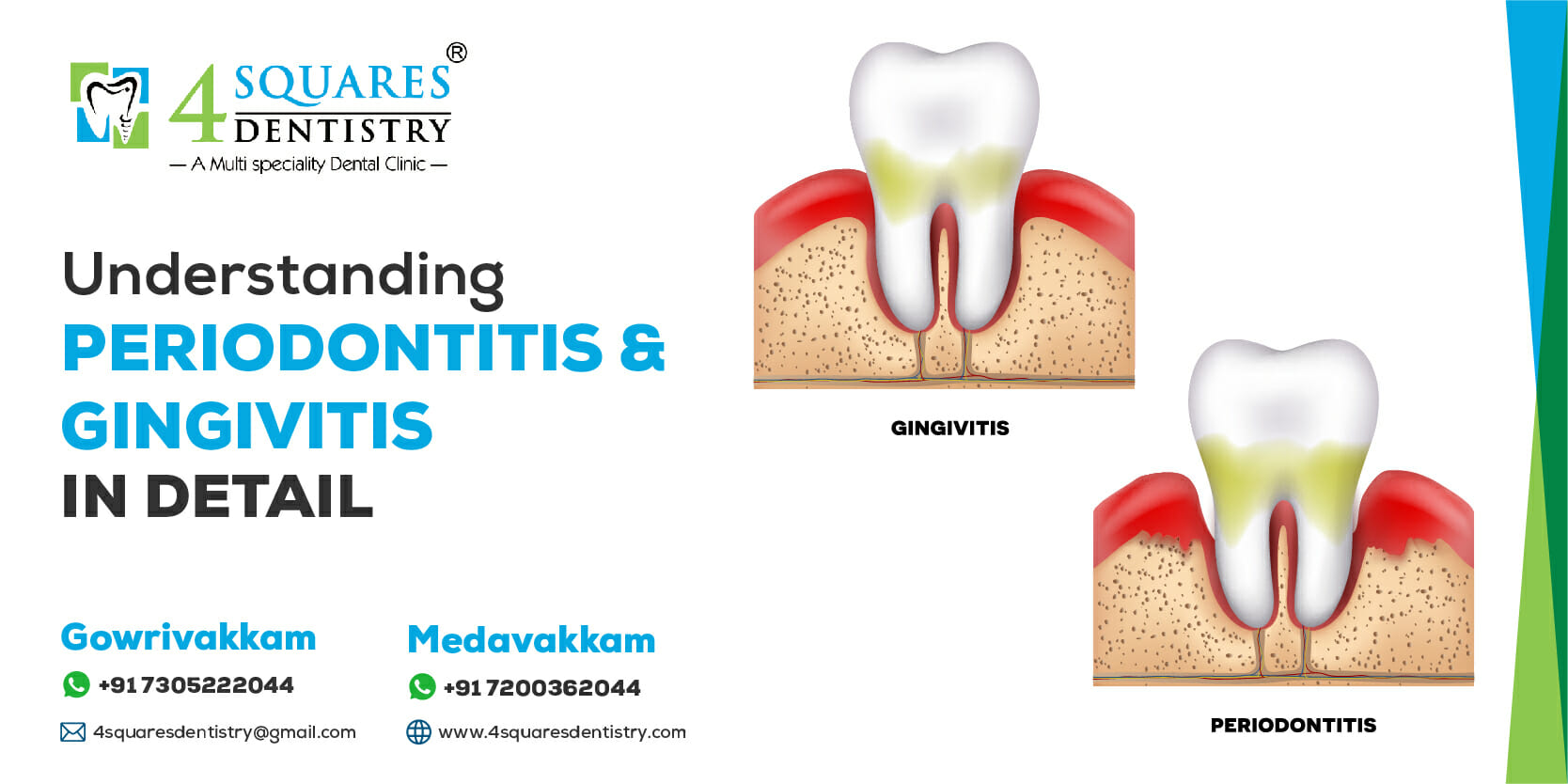
Gum diseases are of two types: Gingivitis and Periodontitis. Very often, people mistake these diseases to be the same. Both diseases affect the gums. However, some characteristics differentiate them.
An in-depth explanation of each disease will help you understand the details.
What is Gingivitis?
Gingivitis is a more common and milder form of gum disease. It is caused by the accumulation of plaque in the areas between the teeth, leading to inflammation of the gums. Plaque is a sticky, odourless, colourless film that constantly forms on your teeth when saliva mixes with food and fluids.
Dental plaque starts forming on the teeth a few hours after food intake. This sticky fluid contains bacteria, which is why it is so important to brush your teeth at least twice a day. Improper brushing leads to plaque accumulation, which leads to gum diseases.
Signs and symptoms of Gingivitis
Healthy gums are pale pink, firm to the touch, and fit snuggly around each tooth. However, when Gingivitis sets in, your gums exhibit the following symptoms:
- Redness and swelling
- Puffy gums that bleed easily
- Random bleeding from the gums
- Bad breath
- Discoloured teeth
- Receding and tender gums
Despite irritated and bleeding gums, gum recession does not occur until later stages of periodontal disease and tooth loss.
Methods of treatment for Gingivitis
The main objective of treating Gingivitis is to minimise inflammation and curb the disease from worsening further. The treatment option includes:
- Maintenance of oral hygiene through practices such as brushing and flossing.
- Professional dental cleaning to remove plaque and tarter.
- Use of mouthwash containing chlorhexidine to curb oral bacteria.
- Fixing dental restorations that contribute to Gingivitis.
What is Periodontitis?
Periodontitis is a more serious form of gum infection that occurs due to the accumulation of tartar on the teeth, close to the gum line. Tartar is a hardened plaque that is rough, porous, and difficult to remove. Periodontitis can destroy the gum tissues and the underlying bone structure that support the teeth. Left untreated, it can result in irreversible gum damage and tooth loss. The main reason for Periodontitis is very poor oral health and hygiene. This gum disease shows characteristic symptoms such as:
- Swollen and severely bleeding gums
- Sensitive and tender gums
- Bad breath
- Loose teeth
- Receding gumline
- Teeth that change positions
- Pain and sensitivity during chewing
- Visible gum pockets
Does Gingivitis progress to Periodontitis? Yes, it does. Untreated Gingivitis leads to more accumulation of plaque. When the bacteria in the plaque release toxins, it leads to severe inflammation. The inflammation, in turn, triggers a chronic inflammatory response, which destroys the gums and bone tissues.
The damaged gums pull away from the teeth, creating gum pockets that are very conducive for bacteria to cause more damage. As the tissue damage worsens, the gum pockets deepen, causing the teeth to loosen and drop off.
Treatments for Periodontitis
Periodontitis is advanced gum disease. Hence it requires more aggressive treatment methods than those meant for Gingivitis. As always, prevention is the key to staving off periodontal diseases. However, with Periodontitis, your dentist may opt for surgical or non-surgical treatment methods, depending on the severity of the disease.
Non-Surgical Treatments
- Scaling- To remove tartar and plaque accumulation from your teeth.
- Root planing- To discourage the further buildup of tartar and remove bacterial byproducts that contribute to the inflammation.
- Antibiotics- To control infection and eliminate the harmful oral bacteria that worsen the condition.
Surgical Treatments
Surgical treatments may be the only choice to treat advanced stages of Periodontitis. Your dentist may suggest:
Tiny incisions are made to lift back the gum tissues and expose the roots for more effective scaling and root planing.
Bone grafting
Small fragments of your bone or synthetic bone are attached to hold your tooth in place and prevent tooth loss.
A small piece of tissue is removed from the palate and attached to the affected gums. Sometimes tissues from another donor source may also be used.
- Guided tissue regeneration
A bio-compatible fabric is attached between the existing bone and the tooth to prevent excessive tissue from entering the healing area. This treatment promotes the healing and regeneration of bone tissues.
- Tissue-stimulating proteins
A special protein-rich gel is applied to the damaged tooth root to stimulate the growth of healthy bones and gum tissues.
Causes & Risk Factors of Periodontal Diseases
The main culprit behind Gingivitis and Periodontitis is poor oral hygiene practices. Improper brushing and flossing lead to residual sugar and carbohydrates in your mouth leading to plaque accumulation. The bacteria in the plaque feed off the residual sugars and release waste byproducts that can irritate your gums and cause inflammation.
There are additional factors that cause gum inflammation, such as:
- Prolonged medication intake reduces the formation of saliva, which normally helps clean the teeth and control bacteria.
- Intake of excessive carbohydrates and sugar-rich foods that contribute to plaque accumulation.
- Vitamin C deficiency leads to unhealthy gums.
- Hormonal changes during puberty or pregnancy that make gums more susceptible to plaque-related inflammation.
The contributing risk factors that worsen Gingivitis and Periodontitis include:
- Smoking and chewing of tobacco
- Genetics
- Substance abuse
- Chronic medical conditions
- Cancer-related therapies
- Steroid intake
- Naturally misaligned teeth
- Stress
Prevention Of Gingivitis & Periodontitis For A Lifetime
Consistent oral hygiene practices are the only simple ways to prevent Gingivitis and Periodontitis. Good oral hygiene can prevent the formation and accumulation of plaque. Without plaque, there is no risk of any gum disease.
All you need to do is:
- Brush your teeth twice a day
- Floss once a day
- Avoid cigarettes and tobacco
- Eat a well-balanced diet
- Visit your dentist regularly
Gingivitis is reversible, and the early stages of Periodontitis are easier to treat and control. In both cases, you need to maintain oral hygiene and make dental visits a part of your annual routine.
To schedule your dental appointments at 4 Squares Dentistry, contact us today!